Some of us can use our gardens if the weather is warm enough, at the moment it isn't so we are not missing much from the sunshine outdoors point of view.
I dont know about naturist clubs but most swimming pools are closed. I hope Naturist clubs are following the government recommendations and closing.
Nude Rambling is a possibility as long as you dont do it in a group, only go with your own family keep it down to small numbers. Keep away from other ramblers and if you need fuel to get to the ramble, wear gloves at the pump and the checkout.
Be safe everyone and take this problem seriously. Keep 2 metres between you and anyone else and remember anything you handle outside the home could have been handled by someone carrying the Virus so wear gloves outside and wash your hands regularly. Do not rely on cheap face masks, the spaces between the weave is bigger than the virus so it can get through.
Many people use the internet and social media to obtain their information about COVID-19, often just called coronavirus. Some of it is correct, much of it is not. As an epidemiologist with over 40 years of experience including seven years working for the World Health Organization, I will try and sort out what we currently know. However, this is a changing feast with new publications every day on all aspects of COVID-19.
COVID-19
Viruses are parasitic in that unlike bacteria, they can only reproduce inside a host cell, whereas bacteria can reproduce anywhere. However, virus particles can survive on surfaces. Viruses can infect all species of animals, and can even infect bacteria. All viruses consist of a core of either RNA or DNA, surround by a fatty coat. RNA viruses cause diseases like influenza, ebola, hepatitis, measles, and HIV. They mutate more easily than DNA-based viruses.
Viruses are nearly always much smaller than bacteria. For example, the bacteria that causes smallpox are about 300 nanometers in diameter, compared to 120 nanometers for coronavirus. To put that in perspective, that makes a coronavirus particle about one 2,000th the size of a grain of salt.
COVID-19 has spikes coming out of it so that it looks like a crown — hence its name. It is these spikes that attach to receptor sites in the lining of your throat, nose and eyes.
Risk factors for COVID-19
In the vast majority of people, a COVD-19 infection results in similar symptoms to the common cold or an influenza. However, some people have a much more severe disease that can end up with multiple organ failure and death.
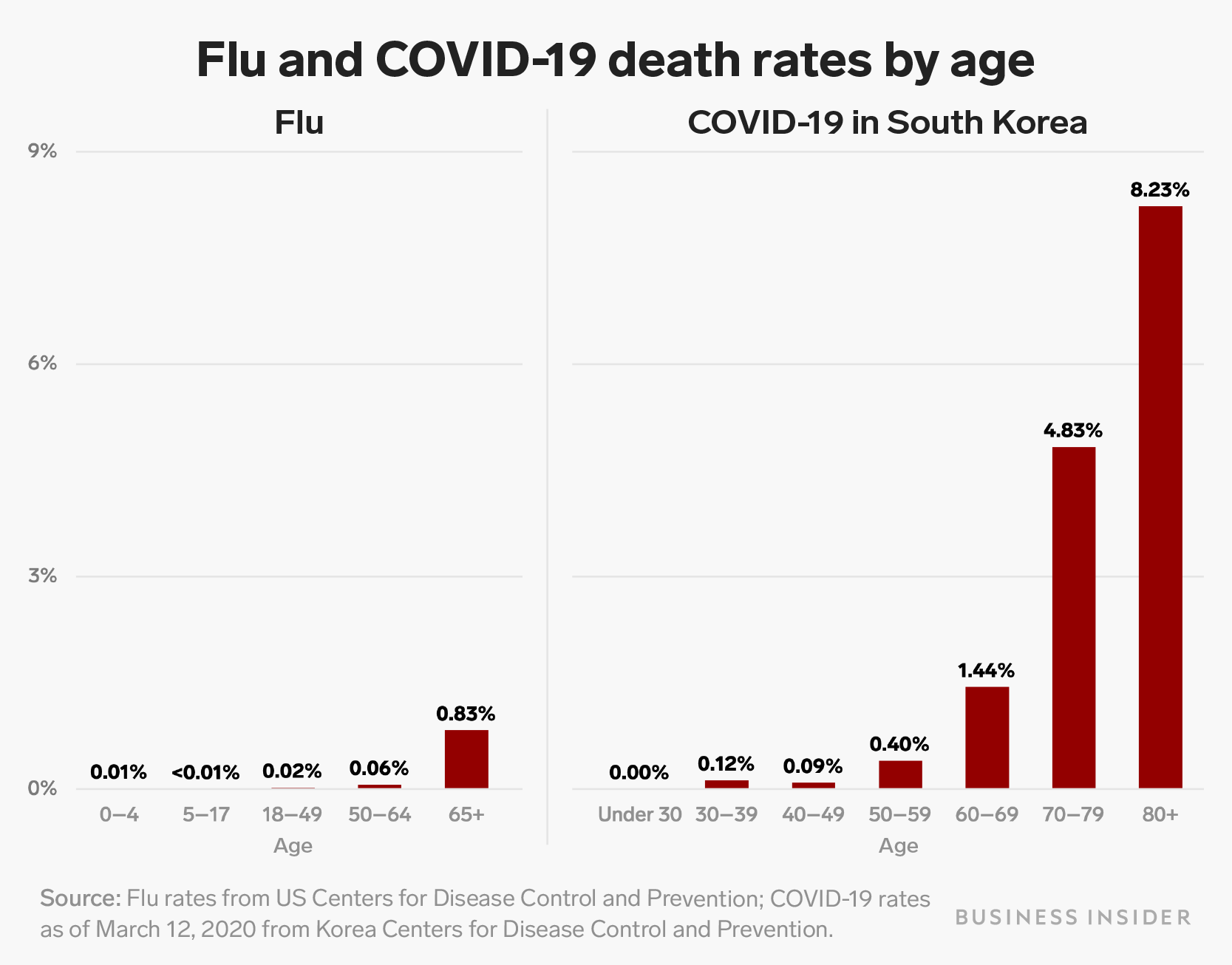
Age is the dominant risk factor for poor outcome as you can see in the above chart, especially in those over 80. Our immune system deteriorates with age, and older people are less able to fight off the infection with their own immune response. On top of that, most elderly people have other chronic conditions that can also increase the severity of the infection. However, although much rarer, younger people (including children) can get very severe infections even without any other underlying condition.
Chronic conditions such as diabetes, hypertension, COPD, asthma and cancer appear to be risk factors. In fact any condition that impacts on your lungs or impairs your immune system puts you at higher risk. However, we are still unclear exactly which specific conditions imply greater risk, and are awaiting more data from China and elsewhere. There is also some controversy over whether some of these do in fact increase risk. If you are on a medication that may impact on your immune system, such as corticosteroids for asthma and rheumatoid arthritis, chemotherapy for cancer, or medication for hypertension, the best advice is to speak to your medical consultant or GP before considering coming off them during the epidemic.
There have been reports published from Chinese researchers that those with blood group A are both at higher risk of infection and of a more severe disease. However, I would like to see this repeated in other studies before I accept it as being correct.
At this time, there is no evidence that pets can spread COVID-19 or that they might be a source of infection.
There is also no evidence that temperature or climate impacts on risk.
Prevention measures

Because the virus particles are so small, they will pass straight through a standard surgical face mask. There is therefore no benefit to be gained from wearing one if you are well. However, if you are sick, then the majority of the particles that you expel when you sneeze or cough are in fact fairly large virus-containing water particles that won’t go through the mask, and therefore wearing one when you are infected will make it less likely you will infect others. It is therefore recommended that infected people, and those who look after them, wear surgical masks.
Doctors and nurses looking after sick patients wear special masks called N25. They are much finer than surgical masks, and can block out even the very small virus particles. But they must be properly fitted to your face and are uncomfortable to wear for long periods of time.
Social distancing is something we should all be doing until the epidemic is over. By that I mean try to avoid coming into close contact with other people, unless it is essential. If you can work from home, you should be doing this now.
The best way to avoid infection is by constantly washing your hands with soap, detergent or a strong alcohol based sanitiser which is at least 60% alcohol. These break down the fatty outer coat of the virus, causing it to die. There are plenty of videos on how to wash your hands properly, such as this one:
Also, regularly clean down and disinfect surfaces that are frequently used like television remote controllers, door handles and counter tops and toilets. This is especially important if you have someone who is sick in the house. First clean with soap and water, then disinfect with hospital grade disinfectant. Make sure that you wear gloves when you do this.
There has been a lot of discussion about whether or not you should pull children out of school. This is a difficult one. Countries like Singapore have kept schools open, and are managing quite well. The current thoughts are that children do not appear to be a major factor in the transmission chain, and the disruption to their schooling might seriously affect them. Each parent will have to make up their own mind about this. I would stick to Government advice.
There are many research groups around the world developing vaccines against COVID-19. Early human trials have already begun in the USA, and an Australian group believe that they can get their vaccine into major production by the end of the year — so hang in there!
Symptoms of coronavirus
Treatments
Likely course of the epidemic
How long the epidemic lasts is based on three important numbers used by epidemiologists . The first of these is called R0 (pronounced Rzero). R0 is the average number of people each infected person infects. Based on data from China and a cruise ship, we are pretty sure that R0 is about 2.5, that is each infected person on average infects 2.5 other people. While R0 is greater than 1, the epidemic will keep increasing. If we can get R0 down to 1, it will become endemic, that is it will be permanently in the population grumbling along at a low level. However, if we can get R0 below 1, the epidemic will die out.
Naturally therefore, all public health measures are designed to try and reduce R0 to below 1. How do we do this? Well first and foremost, we vaccinate the population against COVID-19 — however, this will not be available for a few months.
Secondly, those who contract COVID-19 will become immune and therefore cannot contract the disease again (there has been much discussion about how much immunity you get after contracting the disease), but it looks as those most recovered people will have immunity.
Finally, we can adopt measures such as contact tracing of those affected, quarantining, social distancing, closures of schools, universities and public gatherings. All of these will help reduce R0. By undertaking these measures, we will probably not affect the overall number of people infected, but we will spread out the infections over a longer period of time, allowing our health services to cope better. This approach has been widely discussed on social media as “flattening the curve”.
The next important number is how long we think someone is infectious for. Again, based on the Chinese and cruise ship data, we think it is about 5 days.
Herd immunity
The final crucial number is herd immunity. If enough people in the population have recovered and are immune, or are vaccinated, R0 is driven below 1. Herd immunity is the percentage of the population immune to the disease needed for the epidemic to die out. The formula for herd immunity is actually quite simple:
Herd immunity = 1- (1 / R0). So if R0=2.5, herd immunity= 1–0.4 = 0.6.
In other words, when R0 is 2.5, we need 60% of the population to be immune for the epidemic to die out. If we could drive R0 down to 1.5, herd immunity would be achieved with only 30% of the population having recovered from the illness and thus being immune.
We can use these parameters to do some very simple modelling.
Let’s start off with 100 people infected on Day 1, and R0=2 (because many of us are practising social distancing).
By Day 5 we will have 300 people infected, by Day 10 it will be 900, and by Day 30 it will be 72,900 — so you see how quickly the epidemic can spread, and why R0 is so important.
At the same time, when enough of the population have recovered and become immune, the epidemic will die out.
Therefore, you can see that the next 3–4 months are critical in terms of the demand on our health services, and that by August/September we should start seeing the epidemic subsiding due to herd immunity.
Where to get credible information
The are thousands of articles, blogs, news reports and tweets out there about COVID-19. Apart from that, there is an exponential growth in the number of papers published in medical journals about COVID-19. I suggest that you ignore much of what you see in social media — it might or might not be true. I suggest the following websites as credible sources of information.
In conclusion
With such a rapidly changing scenario, it is clear that there is much we still don’t know about Covid-19, and how long it will take for clinical trials of drug treatments and vaccination to be completed. In the meanwhile, I will update this blog on a daily basis to bring you any strong evidence about risk factors and treatment.
WRITTEN BY










No comments:
Post a Comment